Here's your guide to knowing when it is time to see a doctor about your period
Menstrual pain is a subjective experience - everyone is different. These differences have also caused a great debate around menstruation. Are period cramps really supposed to be painful - or this painful? What is a ‘normal’ amount of period blood to have each month? Is it normal that my period changes month to month? Menstruators across the globe are left wondering either alone, or discussing amongst their communities if their experience is valid, typical, or ‘normal’.
From abdominal cramps to backaches, pain and discomfort are frequent occurrences during menstruation. However, there are times when pain is your body’s way of letting you know something bigger is off.
How do I know if my period cramps are normal?
Period pain is caused due to contractions of the uterus. Changes in your hormones as well as the shedding of your uterus cause more contractions. All this (and so much more!) takes place at the same time, resulting in the release of prostaglandins, causing stronger contractions.
These pains are the lighter cramps or discomfort we often experience the few days leading up to our period, along with period days 1 and 2. Typically, light rest and a hot water bottle can be enough to soothe this pain.
When are period cramps not normal?
If your cramps are stopping you from going to work, school, seeing friends, doing sports, or anything else in your life is a sign something is off. In short, extreme pain which disrupts your normal day is always a sign that something might be amiss.
Since pain is subjective, describing it universally is challenging. Most menstruators are used to having some pain or discomfort associated with their period. However, throughout our lives, menstruators have been led to believe that menstrual pain is a normal part of life; that pain, not light discomfort, is part of being a girl/woman/ person who menstruates. This has led most menstruators to be capable of sustaining high thresholds of period pain because it is simply the norm.
When should I worry about my period?
Another flag is that any period pain that is out of your normal should prompt immediate attention. For example, if it is typical for you to get light cramps, or have one bad day of cramping, but this month you have been in more pain than normal, you should consider seeing a doctor. Other red flag signs that you should consider:
- Being bedridden for days during your period
- Pain that doesn’t subside with OTC painkillers
- Vomiting or nausea
- Intense pain in the back, hips, and thighs
- Dizziness
- Diarrhea associated with the crampy pain
- Intense period pain lasting for more than two days per cycle
It often takes more than one cycle for a menstruator to assess whether their pain is above their average pain threshold. This is why everyone should keep a journal in their agenda or phone that keeps track of your period.
Is it normal that my period is worse some months?
Primary menstrual pain, where no underlying cause for the pain has been sourced out, is observed in about 90% of menstruators. Yet, it is so scarcely reported. A reason could be the limited understanding in assessing menstrual pain.
Studies have shown that among some menstruators there is an increase in the number of prostaglandins produced. This is a common cause for what is termed primary dysmenorrhea (painful menstruation)
Other factors that can contribute to painful menstruation are:
- A uterus that is tilted backward (retroverted uterus)
- Family history of painful menses
- Early menarche (first period)
- Lack of physical activity
- Increased stress
- Lifestyle habits such as smoking and consuming alcohol
These can be contributing factors and do not imply that they should result in painful periods. Primary menstrual pain is what is referred to as a “diagnosis of exclusion”. This means once other possible causes for menstrual pain are ruled out, that painful periods are to be considered primary dysmenorrhea.
When should I see a doctor about my period?
Period pain due to an underlying medical condition is termed secondary dysmenorrhea. Menstruators who have secondary dysmenorrhea have menstrual pain that progressively worsens with each cycle. When you think back on your experiences of menstruation, you can note that your periods have gotten more painful.
This menstrual pain in most cases is directly related to something that is affecting any one of the pelvic organs, such as the uterus, ovaries, or vagina. While there can be an endless list of possible causes, we will discuss a few common ones to get you started. If you have more questions, you should talk to your doctor!
What is endometriosis?
Of late, endometriosis is being cited as a frequent cause of menstrual pain. The number of cases is increasing, primarily since the uncertain signs of endometriosis were previously ignored. With endometriosis, the uterine endometrium lining is found in areas outside of the uterus. These include the fallopian tubes, ovaries, abdominal organs, even the vagina, and rectum. Based on their location menstrual pain can also result in significant abdominal pain and contraction. Pain during sex or defecation should also hint at endometriosis.
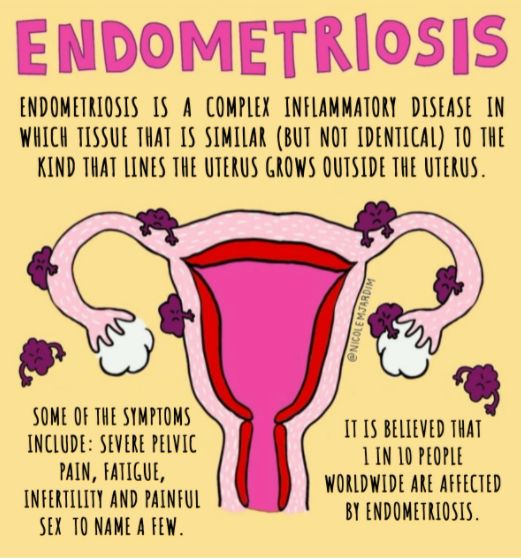
Picture 1: Image Credit: @nicolemjardim
During my years of discussing gynecological health with menstruators, many have come forward with obscure signs for endometriosis such as uncomfortable bloating during their periods. Some experienced only nausea. Many relayed that they received a diagnosis of endometriosis many gastro visits later. Listening to these stories made me understand that for each menstruator it is crucial to time the rise of symptoms. Marking down variations in both location and intensity also eases the diagnosis process.
What is pelvic inflammatory disease?
Pelvic inflammatory disease (PID) is an infection anywhere in the reproductive tract that can potentially result in inflammation which can cause menstrual pain. Most of these infection sources are the common causes of STIs. The most frequent sign of underlying PID is a pain when light pressure is added to the pelvic region. During a vaginal exam, a healthcare provider might also try to create this pain as a test for PID. You will see signs of PID through vaginal discharge and pain during sex. Vaginal discharge can either be thick, watery, or have a foul odor depending on the type of underlying infection. When PID is insufficiently treated or recurs it can cause recurrent menstrual pain.
What are fibroids?
Similar to endometriosis, fibroids have long been underdiagnosed as a cause of menstrual pain. This is primarily due to the evolving series of symptoms based on the size of a fibroid. A menstruator often pushes the initial signs of underlying fibroids aside as common cramps until they have grown to a significant size. In addition to menstrual pain, menstruators may experience pelvic fullness, pain during intercourse, and heavy periods.
In many countries, especially developing nations such as mine, India, fibroids are common, but rarely treated. Many menstruators have reported debilitating menstrual pain, but due to the volume of patients doctors see, fibroids often go untreated. I have also noticed that there is a strong reluctance toward getting fibroids surgically managed. This is often due to the minimal knowledge of post-op care. However, overall, fibroids are a treatable form of menstrual pain.
What is Polycystic Ovarian Syndrome?
PCOS has a prevalence of about 6 to 15%. It is the most frequent cause of menstrual irregularities and infertility. Menstrual pain with PCOS is insidious, it comes in slowly and can have very negative health consequences if left unattended. Due to the bulky ovaries, menstruators have reported crampy pelvic pain in between periods as well. PCOS is cloaked in stigma across the globe, especially due to telltale signs such as weight gain and hirsutism (excess hair growth in typically male patterns). While treatable, due to limited research on possible causes as well as variants of PCOS, menstruators often suffer for years before they receive a diagnosis.
When to see a doctor for your menstrual pain
Adenomyosis, ovarian cysts, premenstrual syndrome, and abscesses are also possible causes of menstrual pain. This list is not exhaustive, if your periods are painful, irregular, heavy, or changing monthly, as well as if you have unbearable pain, you need to talk to a doctor. No one knows your body as you do, let yourself feel confident talking about health with your gyno or family doctor. Menstruators should follow their initial “gut” instinct when their pain reaches beyond their threshold.
Getting help about period pain
Menstruators around the globe are accustomed to pushing their menstrual pain aside. Due to meeting resistance within healthcare settings, it can often be an additional reason why menstruators are reluctant to receive attention for their menstrual pain.
While many facets of menstrual pain might receive judgment, such as unprotected sex that could cause PID, it is crucial to explain all possible causes when questioned. It doesn’t matter how it has happened or why it is happening, what matters is how you go forward and solve for a healthier body. We put together a helpful guide on how to feel more confident talking about sexual health with your gyno, including sample questions. If at any instance you feel that you are not receiving appropriate care for your pain it would be ideal to consult with another gynecologist.
Once you describe what you are experiencing, it is typical for your primary care provider (PCP) to conduct a thorough pelvic exam along with a vaginal speculum exam. Following this, tests such as an ultrasound of diagnostic laparoscopy might be discussed and used. Ask your doctor to explain the need for these tests, take a moment to jot them down in your notes app or on a piece of paper. We talk about a few of these tips in Abitha’s story about her journey advocating for her sexual health in the UK.
What we define as ‘manageable period pain’ is pain that subsides with rest and a hot water bottle. If you find yourself popping pain killers to take care of your menstrual pain, it might indicate a requirement for medical attention. Tracking your period and the symptoms you experience throughout the month, including the ones you might overlook like bloating and nausea, will help give your doctor a better idea of possible causes.
How can I manage my period pain?
Menstrual pain, even the ones associated with a medical condition, can often be managed through a healthy lifestyle. In my years of advocating for healthy lifestyle changes, many menstruators have often reported changes to their pain after just cleaning out their diet and exercising more often. They added in simple changes, as simple as a 30-minute walk every day, and observed a significant change. It is the activities that have the least friction in the day that often provide the most consistent results. There are also a few period cramp relief ideas here that our founder, Jennifer Vrouvides, swears by.
Picture 2 Image by @natracare
Image by @natracare
Menstruators are also encouraged to ensure they are supplementing their body with vital nutrients. Vitamin B and magnesium, either through diet or supplements, can help navigate through some of the period pain. Dietary changes are known to tackle inflammation and pesky symptoms such as bloating. This can include adding fiber to your diet (green leafy veggies and fruits) and sources of probiotics. Alternative health therapies such as acupuncture have also seen some benefits for those who experience significant menstrual pain.
To bring it to a close, menstrual pain should never be overlooked. Generations have been suggesting that menstrual pain is normal and today we simply know that is not the case. The generations before us did not have the same science, shared experience, and information availability we have today. Management for menstrual pain currently looks like a one-size-fits-all: take pain killers, eat ice cream, and watch TV snuggled with a hot water bottle. However, this shouldn’t be the case, your life shouldn’t be on hold because of your period. If you feel uncomfortable with a certain form of management, or wish to try alternatives, discuss it with your doctor. Speak out about your menstrual pain, until it receives the attention it deserves.
Popular reads on YPC
How to Talk About Your Period With Men
Talking about periods with male friends and co-workers doesn’t have to feel like unleashing landmines.
Read moreWhy and When Did Menstruation Become Taboo?
From the Yukon to Greece, taboos around menstruation have been around for ages and still…
Read moreSocial Media’s Important Role in Reducing Period Stigma
From the explosion of period art, to serving as an activist platform in the menstrual…
Read more